We are sharing with you three undergraduate theses from our students that graduated this year. We had a total of six students completing their theses, you can check the others here.
Identifying Molecular Markers of Progression to Muscle Invasive Bladder Cancer
An estimated 9,000 Canadians are diagnosed with bladder cancer each year making it the 5th most common cancer in Canada, the 12th most common among women and the 4th among men. Most patients are initially diagnosed with non-muscle invasive bladder cancer (NMIBC), which in some cases can progress to muscle-invasive bladder cancer (MIBC). MIBC is associated with a significantly poorer prognosis than NMIBC, and it is unclear why some progress to MIBC while others do not. Thus, a better understanding of the molecular progression of bladder cancer is needed. DDR2 is a tyrosine kinase that functions as a cell surface receptor for collagen and regulates cell differentiation, cell migration, invasion, and proliferation. It is known that an increase of DDR2 is ninety percent specific for muscle invasion in bladder cancer and that DDR2 is overexpressed in MIBC compared to NMIBC. Our results showed that MIBC is associated with an increase/gain of DDR2. With that being said, this project sought to demonstrate that DDR2 can be used as a prognostic indicator for the progression to MIBC and can be used as a therapeutic target preventing progression to MIBC.

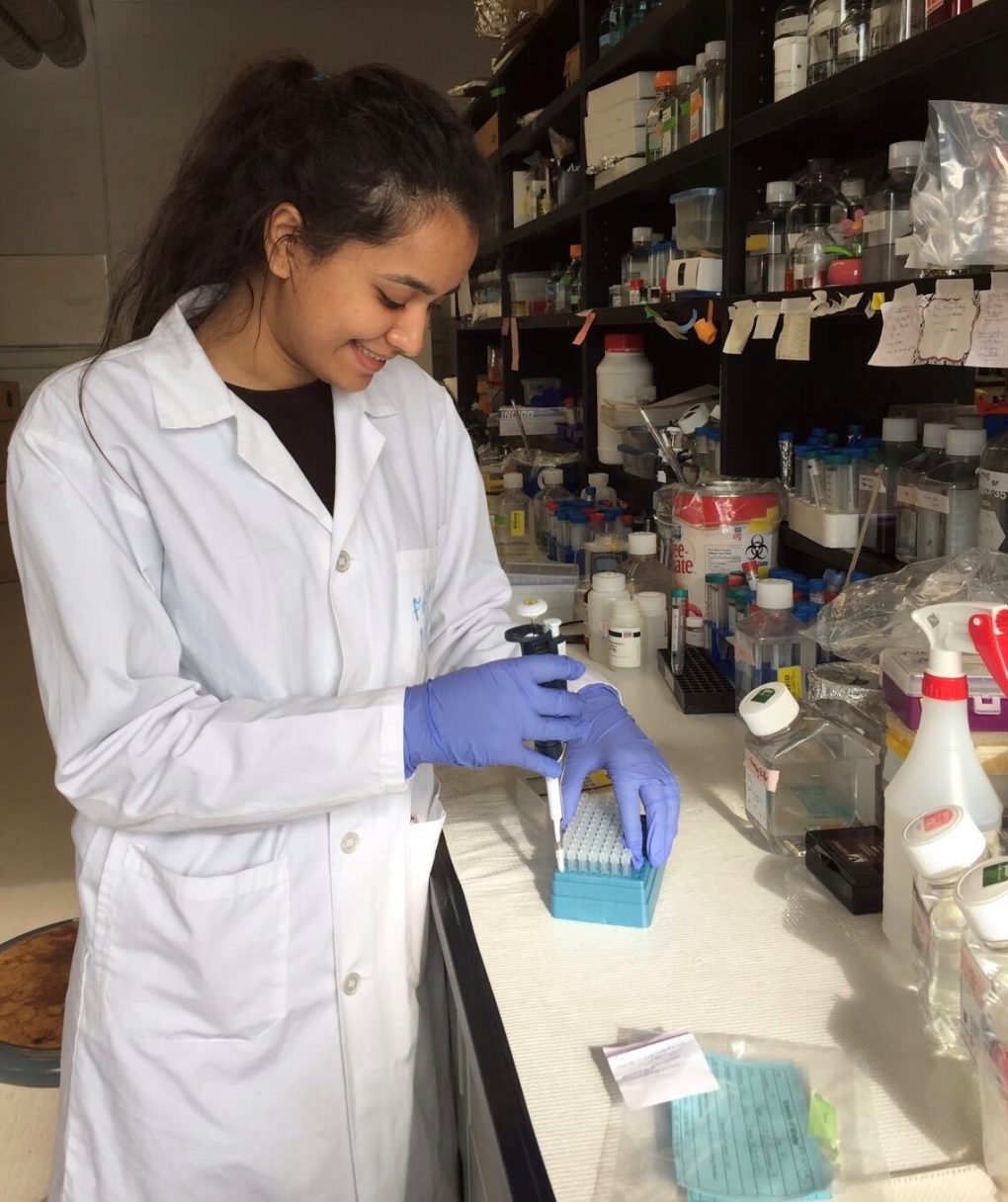
Treatment Timing of Triple-Negative Breast Cancer
Breast cancer is the second highest cause of death from cancer in Canadian women, and triple-negative breast cancer (TNBC) accounts for 10-15% of these cases. Since TNBC lacks three main receptors (estrogen receptor, progesterone receptor, and HER2) that are normally used to target breast cancer, generalized chemotherapy treatments must be used instead. Chemotherapy drugs currently used to treat TNBC include adriamycin (A), cyclophosphamide (C), paclitaxel (T), and carboplatin (Ca). In current treatments, patients receive AC for 4 cycles biweekly followed by T (or T+Ca) for 4 cycles biweekly. Each drug targets various aspects of the cancer cells and causes the cells to arrest in various phases of the cell cycle. This study looked into how the timing and pattern of the administration of the drugs influence the overall results in treating TNBC. To test this, MDA-MB-231 TNBC cells were treated in vitro with one or more of the drugs (AC, T, or T+Ca) at various time-points and the proliferation rate and cell cycle profile of the cells were retrieved using Flow cytometry and Trypan Blue exclusion assay. The results indicated that the pattern of chemotherapy drug treatments that leads to the highest response of TNBC cells was when cells were first treated with T followed by T+Ca. This denotes how the pattern of drugs influences the effectiveness of treatments, and that the order found contains the highest efficiency. The information found may help improve the 5-year survival rate of patients with TNBC and save many lives in the future.
Fatima has completed two theses back to back.
CD44-Selective Conjugated Polymer Nanoparticles: New Theranostics for Glioblastoma Multiforme (2020)
The most aggressive type of brain tumour is Glioblastoma multiforme (GBM). GBM encompasses 17% of all brain tumours, and the median survival for patients does not exceed 15 months. The diffuse nature of the disease and the high level of heterogeneity leads to ineffectiveness of surgical resection and diminished success of established therapies. A novel therapeutic option includes utilizing nanoparticles. My project specifically focuses on the molecular properties of Conjugated Polymer Nanoparticles (CPNs), which are Diketopyrrolopyrrole-based (DPP) CPNs, that are fluorescently labeled with a Hyaluronic Acid (HA) coating. I will first study the CPN concentration-dependent effects on glioma cells in vitro by studying the cell cycle phase accessibility, cell proliferation, death, and metabolic activity. I will investigate the selectivity of targeting CD44, a HA receptor, positive cells by CPNs, comparing CD44+ and CD44- cell populations, separated using Fluorescence-Activated Cell Sorting (FACS), or by using CD44 knockdown. Finally, the bioavailability of CPNs will be assessed using an in vivo Zebrafish system. I will first evaluate any potential toxicity of CPNs on the Zebrafish, and then I will determine the optimal concentration and timing of CPN treatments. I will then investigate the effects of CPNs on xenografted U251 tumours in vivo. This project will enhance our understanding of the CPN-mediated effects not only on the GBM cells but also in an in vivo setting allowing for further development of this therapeutic approach to potentially improve clinical outcomes in patients with GBM.
The Role of the Microenvironmental Landscape in Glioblastoma Multiforme Progression and Therapy Resistance (2019)
Glioblastoma multiforme (GBM) is a type of brain tumour that is categorized as having the highest degree of aggressiveness, accounting for 60% of adult brain tumours with poor prognosis. Despite extensive chemo- and radiotherapy treatments, patients’ relapse. Therefore, a better understanding of GBM biology is crucial to the advent of effective therapeutic interventions. The tumour niche, also known as the cancer stroma, is composed of the extracellular matrix and several types of recruited cells including fibroblasts. Fibroblasts secrete diverse molecules that were found, in other types of cancer, to contribute to the maintenance of the malignant characteristics of the tumour mass. Therefore, we hypothesize that fibroblast activation plays a crucial role in the aggressiveness and progression of GBM. We will first study the characteristics and content of the fibroblast populations in sections obtained from GL261 glioma cell line-derived brain tumours, in comparison to normal brain tissue. We will employ commercially available mouse embryonic fibroblasts to establish co-cultures with GL261 cells in-vitro. Both monolayer and 3D culture models will be utilized to study the activation and the role of the fibroblast component in the control of GBM progression and therapy resistance. In summary, my project will not only contribute to a better understanding of the mechanisms regulating the GBM microenvironment, but it will also identify potential novel treatment approaches.
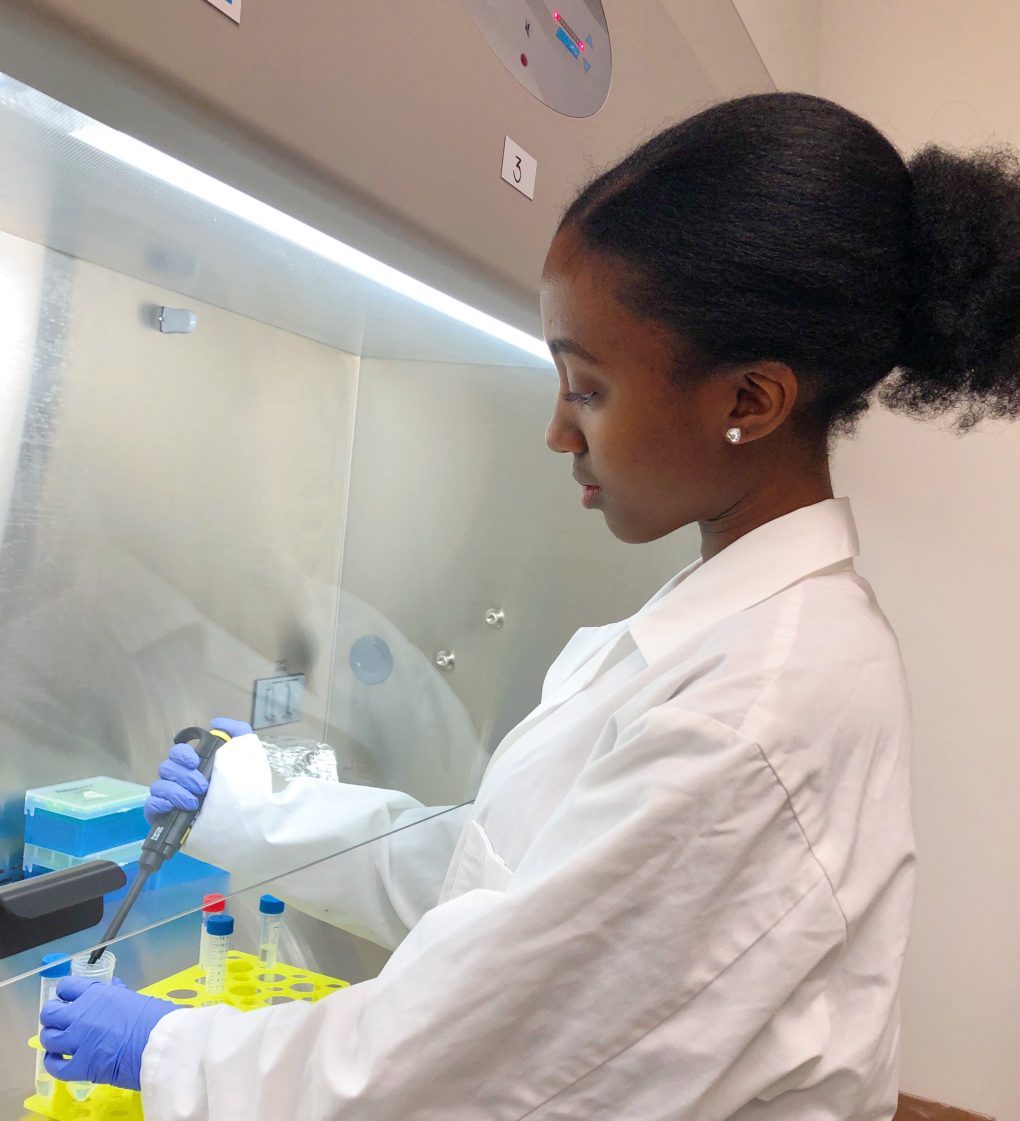
Below, Fatima is sharing with us a little bit of her experience in the Porter Lab.
“Being part of the Porter Lab has meant so much to me and has been the highlight of my undergraduate career. I remember receiving Elizabeth’s email that I had been accepted into the lab after completing an interview during Winter 2017. I was simply over the moon! I started my journey in the lab by helping out with lab maintenance and interacting with several students at different stages in their careers. This gave me insight into what really goes on behind the scenes in a research setting where everyone is a team player and serves an integral role in the overall success of the lab – whether this is through baking filter tips for an RNA extraction or by offering feedback when your IHC doesn’t work. With each semester, I began to appreciate the intricacies of research even more. I greatly admired the determination, grit, and hard work that my fellow lab mates displayed. All these factors and qualities that I gained from my lab team were traits that I knew would help me in my thesis and future career. When I started my thesis, it was definitely a steep learning curve, but I was eager to continue learning and knew that I had my lab team to support me every step of the way. The lab’s continuous support led me to complete two theses featuring projects that I am very passionate about, and which taught me so much about the vast and extensive field of GBM research. I knew how debilitating this disease could be on a personal level as I grew up in an underserved community and witnessed this disease affecting several of my family members. The perseverance of my lab team and knowing that there are so many individuals involved in cancer research is very reassuring and gives me so much hope for those who may be affected by this disease.“