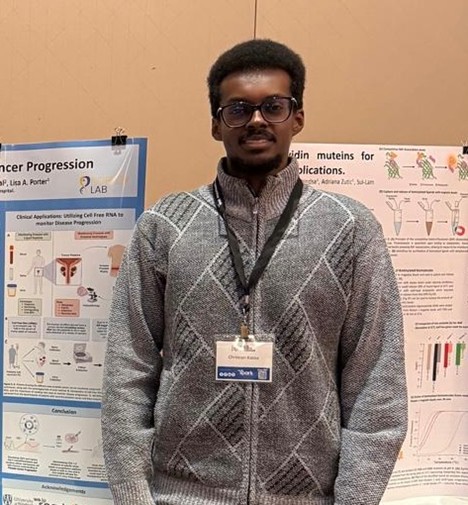
Christopher Jaworski
Being part of the Porter Lab family was one of the most amazing and rewarding experiences of my undergraduate studies. It offered far more than experimental training – it provided a supportive, intellectually stimulating environment where I learned to think critically, troubleshoot experiments, and develop my intrapersonal skills, which will help me in the real world. From the beginning, I was welcomed into a community that values both scientific excellence and personal growth. Whether it was executing the experiment, analyzing data, or collaborating with your lab peers, every task contributed to my development as a researcher. The most important thing I’ve learned during the whole experience is the value of perseverance. You are bound to experimental errors that may alter your results, but you have to see these setbacks as opportunities to rethink and improve, not as failures.


My project focuses on determining the potential of the CDK1/2 inhibitor Dinaciclib as a therapeutic direction for prostate cancer (PC). Adenocarcinoma prostate cancer (AdPC) represents 95% of all PC cases and has several treatment options available, such as surgery, chemotherapy, and hormone therapy, like androgen deprivation therapy (ADT). ADT works by blocking the production of androgens in the body, such as testosterone, to reduce the proliferation of prostate cancer cells. However, some patients do become resistant to ADT, leading to treatment-resistant populations of PC to emerge, called castration-resistant prostate cancer (CRPC). CRPC has a median-survival rate of 1-2 years and is much more aggressive than AdPC. A common treatment method used for CRPC is AR inhibitors, which block the activity of the androgen receptor (AR) outright to slow the proliferation of the prostate cancer cells. However, patients can also become resistant to this form of therapy, and differentiate into a treatment-resistant form called neuroendocrine prostate cancer (NEPC). NEPC is the most aggressive and deadly subtype of prostate cancer, and has a 7-month median survival rate. Furthermore, the downregulation of prostate-specific membrane antigen (PSMA), an important detection target, and AR in the transdifferentiation to NEPC further contribute to the poor prognosis of this type of cancer. Our lab proposes targeting the cell cycle to slow the proliferation of prostate cancer, using a CDK1/2 inhibitor named Dinaciclib. My project uses three prostate cancer cell lines to test the efficacy of Dinaciclib in vitro in stopping the proliferation of prostate cancer cells: LNCaP-FBS, an AdPC cell line, LNCaP-CSS, a CRPC cell line, and NCI-H660, an NEPC cell line. My project also uses zebrafish as an in vivo model to test Dinaciclib’s effect on tumour burden, where zebrafish have been injected with prostate cancer cell lines and treated with Dinaciclib. Zebrafish are a viable model for prostate cancer because they develop rapidly, have transparent embryos, which makes them easy to see under a microscope, and also lack an immune system within their first 10 days of life, decreasing the chance of rejection if they were to be given human cells.
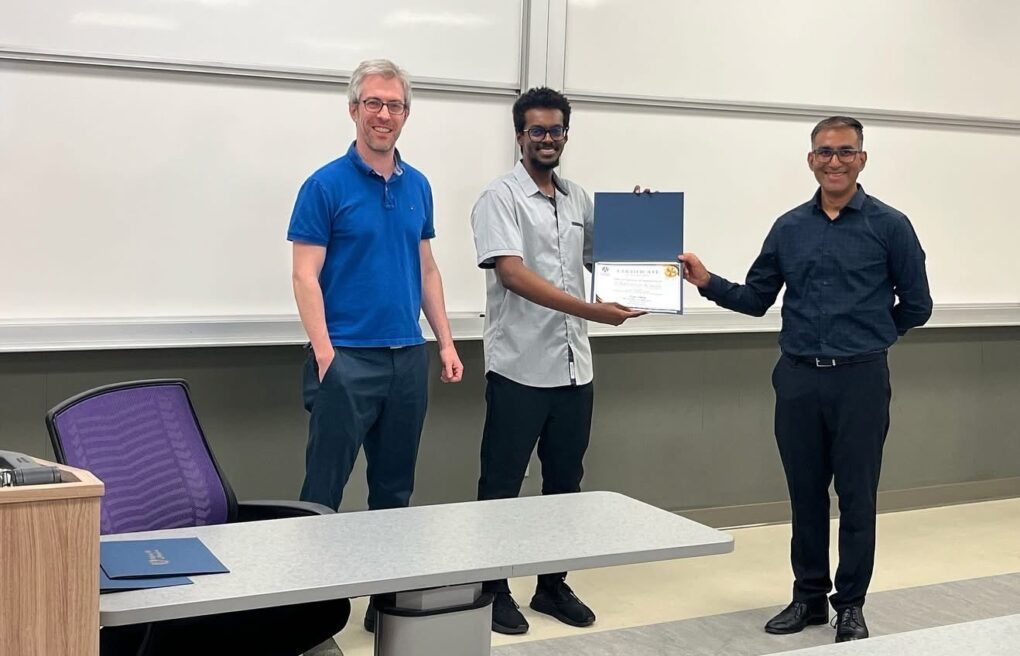
My time in Porter Lab has been one of the most important and fulfilling experiences of my life because it has allowed me to grow not only as a scientist but also as a learner. I would like to express my sincere gratitude to my supervisors Dr. Lisa Porter and Dr. Elizabeth Fidalgo da Silva, as well as PhD and master’s students for their mentorship, encouragement, and guidance in developing my research ability. I wish the best of luck to the next group of thesis undergraduates!